MEDICAL INFORMATICS : ORIGIN, NEED AND ITS CAPACITY TO REVOLUTIONIZE THE HEALTHCARE INDUSTRY
Dr. Surender Gaddam
Invited Guest Article
Medical Informatics (MI) is an interdisciplinary study of information science applied to medicine and health care. It is a branch of science or a developing body of knowledge and a set of techniques concerning the organizational management (acquire, store, analyze, maintain, retrieve, communicate, display and apply) of information to improve patient care, education, medical research, and administration by accurate, timely and reliable decision-making1-3.
The origins of informatics, is based on the science, engineering, and technology of computer hardware, software, and communications. The digital computer has profound implications for the development and practice of clinical medicine. The foundation of MI has "building blocks" of knowledge. They are : information procedure models; information classification principles; information processing methodologies; and functional hierarchical principles of information systems. The structure of MI includes the main knowledge branches and their logical relations. There are four big branches: computer tools and systems methods; engineering equipment and methods; medical fields information systems; and health care management systems4.
MI combines medical science with several technologies and disciplines in the information and computer sciences and provides methodologies by which these can contribute to better use of the medical knowledge base and ultimately to better medical care. MI is the first science that has incorporated all traditional medical disciplines. Implementation of modern technologies, particularly information technologies in medicine, will enable faster data processing; it will reduce expenditures in all branches of medicine (statistics, documentation or documentary etc.) and saves a significant amount of time of the medical staff.
The fundamentals of MI include : communication (telemedicine, teleradiology, patient email, presentations), knowledge management (Journals, consumer health information, evidence based medical information), decision support (reminder systems, diagnostic expert systems, drug interaction) and the management of clinical information (electronic medical records, billing transactions, ordering systems), without which clinicians cannot be truly effective. The tremendous complexity of healthcare and exceedingly huge new information (10,000 clinical trials every year, practice guidelines, recent advances) on daily basis makes it impossible for the clinician to keep abreast of the medical information (knowledge). Though a significant amount of research is conducted (systematic reviews, controlled trials or any other form of evidence), the evidence says that only less than 50% of it is used in practice by the clinicians and other healthcare organizations. This makes MI play a significant role in making the information available to the users i.e., in producing, disseminating, and using the evidence, the essential components for successful evidence based practice.
The current best available valid and reliable evidence says that MI can reduce cost and improve the quality of care by providing safe, effective, patient-centered, timely, efficient, and equitable healthcare5. A clinical decision support system (CDSS) is a software that integrates information on the characteristics of individual patients with computerized knowledge base for the purpose of generating patient specific assessments or recommendations designed to aid clinicians and/or patients in making decisions. CDSS applications assist clinicians and patients with three types of decisions : preventive and monitoring tasks, prescribing of drugs, and diagnosis and management. Shea6 and co-reviewers, in a meta-analysis concluded that the computer remainders were found to improve preventive practices for vaccinations, breast cancer screening, colorectal cancer screening, and cardiovascular risk reduction. In another meta-analysis7 of 33 studies of the effect of prompting clinicians, 25 of which used computer generated prompts, the technique found to enhance the performance in all the 16 preventive care procedures. A study8 concluded computer prescribing of drugs offers potential benefit in such areas as doing calculations and scheduling, drug selection, screening for interactions, and monitoring and documentation of adverse side effects. Computer assisted diagnosis and management is challenging. These systems require an expansive knowledge base covering the full range of diseases and conditions, detailed patient specific clinical information and powerful computation engine. There is no convincing evidence to assess the role of CDSSs in diagnosis.
In a recently conducted randomized controlled trial9 of SPPARO (System Providing Patients Access to Records Online), a patient-accessible electronic patient records (EPR) system at University of Colorado, USA, Stephen E Ross and his colleagues concluded that providing patients with secure access to their medical records using the Internet is feasible and improves adherence which may help assist patients in the self-management of chronic diseases such as heart failure and asthma. Other computerized medical records systems10 proved to be efficient in United States are COSTAR (Computer Stored Ambulatory Record), RMRS (Regenstrief Medical Record System), HELP (Health Evaluation through Logical Processing, ARAMIS (Arthritis, Rheumatism and Aging Medical Information System), CHESS (Comprehensive Health Enhancement Support System), and (SBIR) Small Business Innovative Research. There is no evidence of CDSS or EPR systems in use in India. However, some of them are in testing phase in various private clinics11.
Internet has become the principal vehicle for communication of health information for both consumers and the clinicians. There is enormous amount of healthcare information available online for free. The consumers can access the websites to research an illness or disease, seek nutrition and fitness information, research drugs and their interaction, find a doctor and a hospital, and look for online medical support system. One of the rich sources of healthcare and medical information available on the Internet is MEDLINE maintained by National Library of Medicine, USA. It is estimated12 that 30 percent of the MEDLINE searches are by the members of general public and students, 34 percent by healthcare professionals, and 36 percent by researchers. MEDLINE contains more than 10 million citations and abstracts of articles. While 45,000 journals from different countries are indexed in MEDLINE database, only 45 them are of Indian origin and a lot need to be done to enhance to the international standards to bring up the number. A similar bibliographic database in India is IndMED of Indian Medlars center. Presently, around 80 peer reviewed biomedical journals are indexed in this database and the number is increasing rapidly. Apart from the biomedical journals, an effort should be made to make health information available to the general public through Medlars center. There are many other sources of evidence-based information available worldwide (Cochrane library, National Guideline Clearing House, Agency for Healthcare research and Quality and many more).
It has become a challenge for the practicing clinicians, in terms of their survival of practice until unless they keep up with the present evidence based healthcare (EBH) environment. For those who are very busy in their clinical practice (lack of time), MI is a boon for them as they can access the recent advancements and publications from their office desk with a minimal knowledge of computers and the existing user-friendly systems. Many studies13 worldwide have concluded that the use of MI in the undergraduate and postgraduate education in medical schools has a tremendous impact in preparing the physicians for EBH environment. Working with a laptop in classrooms and laboratories had been proven to be far superior to training at the microscope. Students in medical schools learn to access bibliographic databases (MEDLINE, OVID, Cochrane, IndMED) and clinical guidelines, use handheld computers (PDAs), determine clinical and patient services available, apply knowledge and skills of MI in presentations (PowerPoint), use electronic technologies that support patient care and medical education, utilize EBM in self-directed learning and patient management, and access web sites of health policy. Distance education with live transmission of lectures or prerecorded videos, real time consultations about difficult cases, simulation of surgical procedures, collaborative projects, and virtual exploration of the three dimensional environments are some of the other type of applications of MI in professional education.
MI is widely used in health services, biomedical, and clinical outcomes research. Administrative and clinical data is the backbone for health services research. Computers provide the opportunity of constructing huge databases, and one can access the remote databases (local, national and international) and search for the professional literature through the Internet. It has become a common practice of collaboration among the researchers and research organizations, which is impossible without computers. Peer review and interactive virtual conferences are also an application of Informatics in medical research. Information systems are being utilized in variations research14 to provide an array of potential variables, to provide measures of the variability inherent in these variables, and to assist with the study of the linkages of patient and provider characteristics with interventions and outcomes. Specific implications for medical informatics are in two areas: 1) variable selection and data capture; and 2) delivery of interventions aimed at reducing variation in practice within single or multiple settings. Control of experimental equipment (e.g., Electron Microscope), transfer of large databases between computers for high speed computation and comparisons and enrolling of populations in clinical trials are some of the applications where Informatics are commonly used in clinical and biomedical research.
MI has the capacity to enhance confidence in management of patients not only in urban settings but also in rural physicians. This was demonstrated in a study conducted by Zdanuk S15 and his colleagues using CD based MI in managing HCV patients in a rural area. This approach is of more value than providing similar information in the form of review articles and/or position papers and is suggested by a comparison with the results of a similar study reported by Shehab et al16.
An essential part of health informatics is telemedicine, the use of advanced telecommunications technologies to bridge distance and support health care delivery and education. The modern technology has the capability to capture and transmit textual, audio and video information to distant places that makes its use improve healthcare in rural areas, in the home, and places where the medical personals are not readily available. The health care services could be provided in three categories17 {store-and-forward (collect clinical data, store them, and then forward them to be interpreted later), self-monitoring/testing (enable physicians and other health care providers to monitor physiologic measurements, test results, images, and sounds, usually collected in a patient's residence or a care facility), and clinician-interactive services (real-time clinician-patient interactions that, in the conventional approach, require face-to-face encounters between a patient and a physician or other health care provider)}. In India, some of the teaching institutes (AIIMS, PGIMER Chandigarh, SGPGIMS Lucknow) and corporate hospitals (Apollo (in nine states) and Care hospitals, Hyderabad) are currently linked up using telemedicine application. The first telemedicine link between India and Pakistan was formally opened recently (sep 28, 2023) to facilitate exchange of medical reports and interaction between medical experts of the two countries.
Bioinformatics (BI) is the use of Informatics to facilitate research in biological (especially genomic) sciences. Though both MI and BI seem to be same, they are not. While MI deals with clinical data with emphasis on information systems for patient care, hospital, education, and telemedicine, BI deals with scientific data of molecular biology and biochemistry with emphasis on ontologies, network models etc. The differences between the disciplines are based on differing in historical development, scientific content, and informatics goals. However, a new field called biomedical informatics had been emerged with new advances and approaches in both MI and BI, based on systems biology and Informatics. The clinical decision support systems based on techniques derived from neuroinformatics (NI) and BI have the potential to improve medical diagnostics and will finally lead to a personalized delivery of healthcare. This was evident from a review18 conducted by Weimer and his colleagues in which they concluded that there is a great potential of synergies between BI, MI and NI where techniques are transferred from one of the disciplines to the other (mutual transfer of knowledge and techniques). They found synergies in 1) the modeling of neurophysiological systems for medical therapy development, 2) the use of image processing techniques from medical computer vision for the analysis of the dynamics of cell nuclei, and 3) the application of NI tools for data mining in BI and as classifiers in clinical oncology.
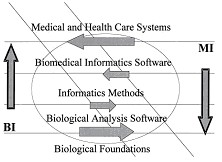
Graphic metaphor of potential synergies and competition between medical informatics (MI) and bioinformatics (BI) indicating directions from current emphases toward increased interactions and the sharing of methods and tools within biomedical
informatics. The diagonal zone represents the area of largest expected complementarities and synergies, while the lightly outlined central oval represents a zone of possible competitive challenges in subtopics of greatest overlap between MI and BI.Collaborations on the Road to Genomic Medicine? Victor Maojo et al. J Am Med Inform Assoc. 2003 November; 10 (6): 515–522)
Artificial intelligence is a sub topic of MI, capable of analyzing19 complex medical data. Their potential to exploit meaningful relationship within a data set can be used in the diagnosis, treatment and predicting outcome in many clinical scenarios. Artificial neural network is the most commonly used analytical tool whilst other artificial intelligent techniques such as fuzzy expert systems, evolutionary computation and hybrid intelligent systems have all been used in different clinical settings. Artificial Intelligence techniques have the potential to be applied in almost every field of medicine. However, there is need for further clinical trials, which are appropriately designed before these emergent techniques find application in the real clinical setting.
The bottom line is that MI with its interdisciplinary in nature, its structure, its simplicity for all medical disciplines to adapt it, its tremendous capacity to improve the quality of medical care (both routine and emergency therapeutic, and preventive) either directly or indirectly, its potential to be used both in urban and rural setting, in tertiary or primary care setting, its capability to make the health services reach the unreached and serve the underserved, its crucial role in health services, medical, biomedical and variation research and its undoubtedly significant role in professional education to prepare the younger brains to work in EBH environment, if implemented in an appropriate manner would revolutionize the healthcare industry (beyond a reasonable doubt) in India very soon.
……………… Enter to Learn and Leave to Serve ………………
REFERENCES:
-
Association of American Medical Colleges, 1986.
-
Charles Friedman, Center for Biomedical Informatics: Introductory Lecture Series, Medical Informatics:Challenges and Opportunities, 1996.
-
Warner, Sorenson and Bouhaddou, Knowledge Engineering in Health Informatics, 1997.
-
Li Z, Mitchell J, Tian A, Rikli A. On the foundation and structure of medical informatics. Medinfo 1995; 8 Pt 2:1265-9.
-
Crossing the Quality Chasm: A New Health System for the 21st Century, July 2001, National Academy Press. Washington D.C.
-
Shea et al. A Meta-analysis of 16 randomized trials to Evaluate Computer-Based Clinical Remainder Systems for Preventive Care in the Ambulatory Setting. J Am Med Inform Assoc 3(6): 399-409, 1996.
-
Balas et al. improving Preventive Care by Prompting Physicians. Arch Int Med 160(3): 301-308, 2000.
-
Schiff DG, Donald RT. Computerized Prescribing: Building the Electronic Infrastructure for Better Medication Usage. JAMA 279(13): 1024-1029, 1998.
-
Ross SE et al. providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: Randomized Trial. J Med Internet Res 2004; 6(2): e12.
-
Medical Informatics for Better and Safer Health Care. Agency for Healthcare Research and Quality.http://www.ahrq.gov/data/informatics/informatria.htm.
-
Open Clinical. Knowledge Management for Medical Care. Diagnostic Decision Support Systems. http://www.openclinical.org/home.html.
-
Lindberg et al. Updates Linking Evidence and Experience. Medicine and Health on the Internet: The Good, the Bad, and the Ugly. JAMA 280(15): 1303-1304, 1998.
-
(Gjerde CL et al. Teaching of Medical Informatics in UME-21 Medical Schools: Best Practices and Useful Resources. Fam Med 2004; 36(January suppl): S68-S73.).
-
Holzemer WL, Reilly CA. Variables, variability, and variations research: implications for medical informatics. J Am Med Inform Assoc. 1995 May-Jun; 2(3): 183-90.
-
Zdanuk S et al. The impact of medical informatics on the confidence of rural physicians caring for patients with chronic hepatitis C viral infections. Fam Pract. 2001 Dec; 18(6): 602-4.
-
Shehab TM, et al. Current practice patterns of primary care physicians in the management of patients with hepatitis C. Hepatology 1999; 30: 794-800.).
-
Telemedicine for the Medicare Population. National Library of Medicine.http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.33002
-
Weimer J et al. Informatics united: exemplary studies combining medical informatics, neuroinformatics and bioinformatics. Methods Inf Med. 2003; 42(2): 126-33.
-
Artificial intelligence in medicine. Ramesh AN, Kambhampati C, Monson JR, Drew PJ. Ann R Coll Surg Engl. 2004 Sep; 86(5): 334-338.