|
Patient Non-Compliance: Where and Why |
||||||
|
|
||||||
|
Where ? |
||||||
|
As is clear from the diagram above, patient non-compliance occurs everywhere and anywhere. Once a patient leaves a doctor's office or is discharged from the hospital, the patient (and his/her family) is primarily responsible for following through the guidelines of treatment laid down by the healthcare provider. However, this also happens to be the venue for patient non-compliance. Patient non-compliance can be in various degrees from missing a few dosages of medication to complete negligence; accordingly are the consequences: health-wise and financial. Typically in non-symptomatic and chronic life threatening diseases like diabetes, hypertension, etc., the tendency for patient non-compliance is very high. In diseases like Arthritis, the incidence of patient non-compliance is very low, since the "symptom" in this case pain, is a constant reckoner. |
||||||
|
Why ? |
||||||
|
Since the whole area of patient non-compliance and disease management is relatively new, no historical statistics are available on the trend. However with constantly increasing healthcare costs, this issue has most definitely come to the forefront. Since this issue also provides substantial economic justification (read incentive) healthcare companies have now become very actively involved in research and innovation in this area. While patient non-compliance is commonly viewed as a "behavioral issue" and is widely credited to omni-present human trait of "forgetfulness", the following statistics may help view its presence with more understanding: |
||||||
|
||||||
|
With nearly 16% of US citizens without healthcare insurance coverage, patient's financial condition is often attributed as a primary cause for patient non-compliance. While this cause can't be completely ruled out, patient behavior has finally been accepted as a primary cause for patient non-compliance. |
||||||
|
This is where the disease management industry has evolved. Modification of patient behaviour and provide them tools to manage their disease better via Patient Education and Real Time Intervention. |
||||||
|
Disease Management: Methods and Tools |
||||||
|
In the US, the current leaders in this industry are companies like American Healthways, Matria, Q-Med, Life Masters,etc. |
||||||
|
Each company has "invented" their own unique method as their claim to fame. However, essentially disease management companies can be classified as :
|
||||||
|
With demand and competition in this industry it is becoming increasingly difficult to find a company, which is purely adhering to any one single method or tool. |
||||||
|
While conventional disease management companies extended the concept of "case management" and re-packaged the same as "disease management". Case management (which is an expensive proposition) was reserved for the critically ill or patients requiring acute care, where the management of the disease required constant medical expertise. |
||||||
|
This included patients have complex surgeries, patients requiring dialysis, etc. However, using the same building blocks of case management, companies such as American Healthways paved the path for disease management. Here they would be manage patients suffering with chronic illnesses such as diabetes, asthma and hypertension which typically don't require acute care if managed properly. |
||||||
|
The two primary differences between case management and disease management are :
|
||||||
|
Conventional Disease Management Involves : |
||||||
|
||||||
|
e.g. A patient may actually get a free glucose meter or a free blood pressure meter or free movie tickets for attending a seminar on management of diabetes or completing q questionnaire, etc. Patients with specific disease and behavior profile would be invited to this seminar and most definitely keeping the patient out of the emergency room once pays for 40 movie tickets. That is the return on investment (ROI) for the incentive program. |
||||||
|
Automated Tools based Disease Management Involves :
|
||||||
|
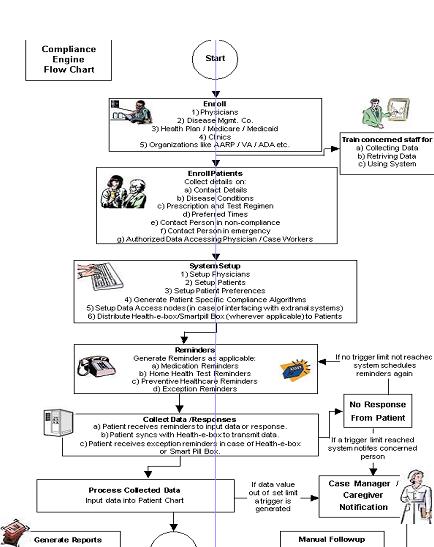
An example is discussed on the next page. The following chart provides the flow for a tool called Compliance Engine powered by PanHealth, Inc.; a Livingston NJ based company creating Automated Tools for disease management. |
||||||
|
|
||||||